What is Osteoporosis?
What is Osteoporosis?
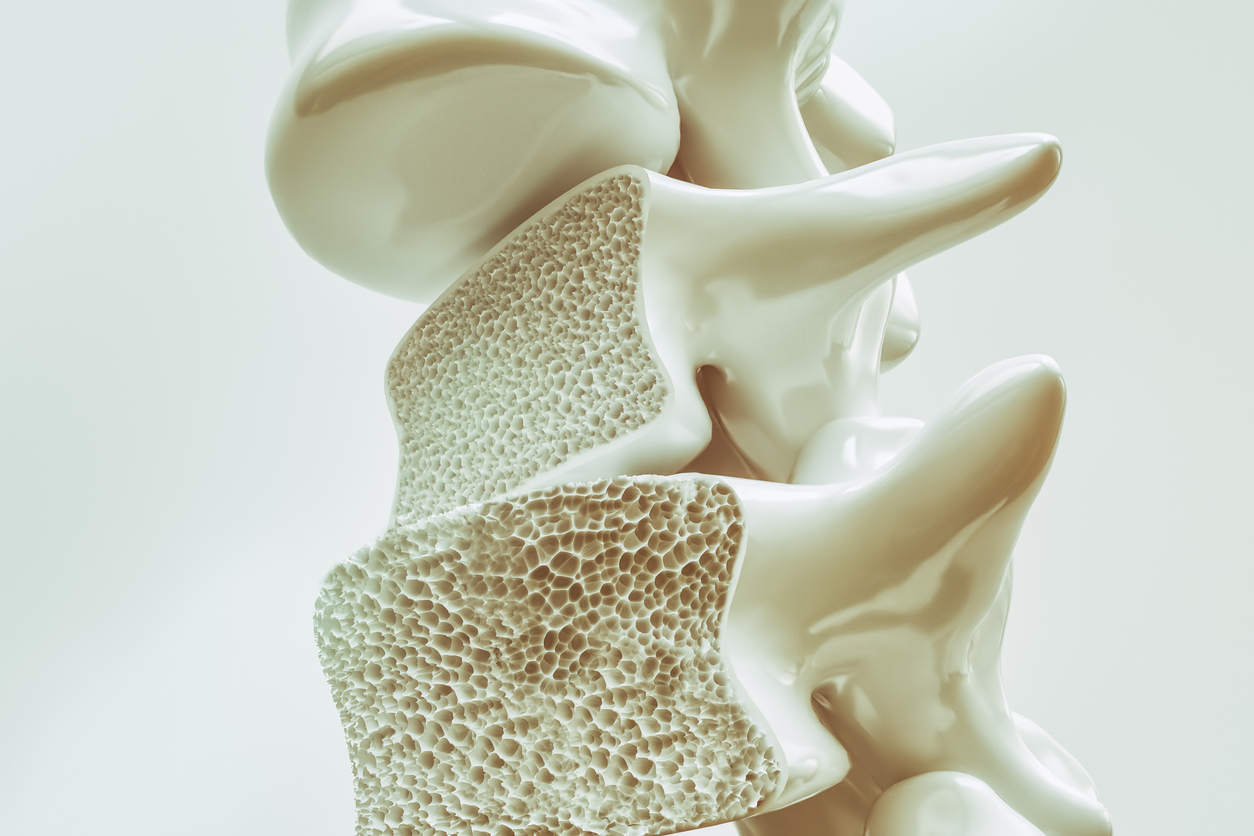
Osteoporosis is a bone disease where bones become weak and frail due to bone loss outpacing the formation of new bone. Nearly 54 million Americans have osteoporosis or low bone mass which leads to bones becoming porous and brittle. With osteoporosis, bone tissue disintegrates, losing minerals and calcium that once made them strong and durable. When osteoporosis affects the bones, there’s an increased risk for bone fracture and bone breakage.
Osteoporosis Causes
Osteoporosis is caused by losing bone mass faster than your body can make new bone mass. The bones in our bodies are living tissue and in a constant process of dissolving and reforming to keep pace with the body’s calcium requirements and to repair any damage. Our bones turnover throughout our lives, reaching peak bone mass by age 30. As we age, however, our bone cells begin to deteriorate while new bone cells form – in a cycle called “remodeling”. In the case of osteoporosis, the remodeling process is hindered when bone tissue dissolves faster than new tissue can keep up. The end result is bones that lose bone mass and density, thus becoming fragile, delicate, and susceptible to breaking and fracturing.
Risk Factors
Age: Bone mass begins to decline after age 30, with most people developing the disease as they age past 50 years old.
Gender: Women have longer life spans, but thinner and lighter bones. As a result, women are 4x more likely to develop osteoporosis than men.
Race: Osteoporosis is especially prevalent in those who are white or of Asian descent.
Family History: Grandparents, parents, or even siblings who have had or have osteoporosis increases your likelihood of developing the disease.
Body Size, Weight, & Frame: Those with smaller body frames have less bone mass than those with larger body frames or body weight. With less bone mass to draw from, the greater the risk of developing osteoporosis.
Low Calcium: Those with lower calcium intake over the course of their lifetime have a higher risk of osteoporosis since calcium is integral to increasing bone density and strength.
Eating Disorders: Restricting food and remaining underweight weakens bone mass and density.
Hormone Imbalances: Those with an overactive thyroid, deficient in estrogen or testosterone, or other hormonal issues may have an increased risk since these imbalances are associated with weakened bone and bone loss.
Sedentary Lifestyle: Spending a lot of time sitting and without physical activity puts your body at risk of developing osteoporosis. Lifting weights and cardio can help protect your bones.
Steroids and Certain Medications: Specific medications and steroids taken over a prolonged period, such as prednisone or cortisone, can affect the bone-rebuilding cycle.
Medical Conditions: Those with rheumatoid arthritis, celiac disease, lupus, cancer, IBD, kidney or liver disease have increased odds of developing osteoporosis.
Smoking & Alcoholism: Tobacco use contributes to weaker bones and drinking frequently can cause bone thinning.
Osteoporosis Symptoms & Signs
Many people do not realize they have osteoporosis until they break or fracture a bone. However, there are some noticeable red flags that may signal the different stages of the disease. These are not limited to but can include:
- Backaches
- Weaker grip
- Receding gums or tooth loss
- Brittle fingernails
- Spine, wrist, or hip fractures
- Neck pain
- Loss of height or sunken posture (may indicate a compression fracture)
- Noticeable hump in the upper back (also called a “widow’s hump”)

Diagnosing Osteoporosis
If you suspect you have osteoporosis or that your bones are getting weaker, your doctor may conduct some of the following tests:
- X-Ray
- CT Scan
- Bone Mineral Density (BMD) test
What is a Bone Mineral Density (BMD) Test?
Also referred to as dual energy X-ray absorptiometry (DXA), is a type of low radiation X-ray test that measures the calcium and minerals in your bones. The results, named your T-Score, is a score based on a healthy bone mineral density of a 30-year old.
The National Institutes of Health (NIH) provides the guidelines for BMD scores:
- A normal score is between 1 and -1
- A low bone mass score is between -1 and -2.5
- A score that indicates osteoporosis is at -2.5 or lower
- Severe osteoporosis is a score of -2.5 or lower with bone fractures
Depending on your results from the BMD test, your doctor may follow up with a few more tests or work to get a treatment plan in action.
Osteoporosis Treatment
Once diagnosed, treatment starts with either treating existing fractures or preventing fractures. While osteoporosis cannot be cured, there are ways to manage the disease everyday to help fortify your bones.
Fracture Treatment
If you have a fracture, your doctor will likely put a cast on the area to hold it in place and allow it to gradually heal. While the fracture is mending, you’ll probably need painkillers or NSAIDs to relieve any discomfort.
Fracture Prevention
There are a number of ways to prevent and treat weak bones and the risk of getting a fracture. A mix of lifestyle changes as well as doctor-ordered treatment options can help manage the disease.
Lifestyle Changes
Diet: Calcium and other minerals help increase the strength of your bones. In your diet, eat foods that are high in calcium and vitamin D like broccoli, salmon, leafy greens, and dairy. If you’re older, aim for an intake of 1,200 mg of calcium each day. While it’s ideal to get your calcium, minerals, and nutrients from food, you can also take supplements. On the flipside, phosphorus can promote bone loss – avoid high-phosphorus foods like red meat, nuts, and foods with added phosphates.

Exercise: Exercise is important for increasing bone density and strength. It’s recommended to exercise at least three times a week for 45 minutes. Weight-bearing exercises are particularly helpful, like running, walking, stair-climbing, weightlifting, or aerobics.
Cut Down on Alcohol: Alcohol contributes to lowering the amount of calcium your body absorbs, leading to bone thinning and weaker bones overall. Cutting down on alcohol and caffeine will help strengthen bones.
Quit Smoking: Tobacco use contributes to decreasing bone density and making you more susceptible to bone fractures and breaks.
Medications
Bisphosphonates: These are the most widely prescribed medications for both men and women, and they work to slow down bone loss by slowing down the cells that deteriorate your bones. The full effects of the medication, or a substantial decrease in bone turnover, should show within three to six months. While there are side effects of bisphosphonates, they’re not common if you take the medications properly. Some examples of prescription bisphosphonate medications are:
- Alendronate (Binosto, Fosamax)
- Risedronate (Actonel, Atelvia)
- Ibandronate (Boniva)
- Zoledronate (Reclast, Zometa)
- Pamidronate (Aredia)
- Etidronate (Didronel)
Discuss the best treatment option with your doctor for your specific case of osteoporosis. If they recommend a prescription oral or intravenous medication, be sure to disclose any other medications or health conditions so your doctor can confirm they won’t interfere with treatment.
Ongoing Support for Those Living with Osteoporosis
Osteoporosis is incurable, but many go on to live long lives through making the appropriate lifestyle changes and managing the disease. If you have osteoporosis, you’re not alone – there are 10 million Americans living with the disease, and another 44 million who are at risk. There’s so many resources to turn to when it comes to finding support in controlling your diagnosis. Below are just a few:
- NIH Osteoporosis and Related Bone Diseases National Resource Center
- National Osteoporosis Foundation: Online Community & Support Groups
- NOF Nutrition Guidelines
- Osteoporosis Worldwide Facebook Support Group
- Mayo Clinic Exercises with Osteoporosis
If you’re having difficulty living on your own with osteoporosis, consider home care services to help you around the house and in your daily life. Open Systems Healthcare can help with our personal care services.