What is Type 2 Diabetes?
What is Type 2 Diabetes?
According to the CDC, there are more than 100 million American adults living with diabetes or prediabetes. Type 2 diabetes is the most common form of the disease, and is typically adult-onset. However, in recent years the number of younger people diagnosed with type 2 diabetes has grown exponentially as well.
Type 2 diabetes affects the way your body processes glucose, also known as blood sugar. Insulin, a hormone made by the pancreas, helps remove glucose from the blood and into your cells so that it can be used for energy. In type 2 diabetes, your body does not utilize insulin properly, resulting in unregulated blood sugar levels. Without that insulin working correctly, too much glucose remains in your blood and not enough reaches your cells, resulting in high blood sugar that could lead to a host of health issues.
There is no cure for type 2 diabetes, but the disease can be managed by taking care of your body and following the proper treatments for your case.
Type 2 Diabetes Causes
Type 2 diabetes progresses when blood sugar is too high or when the pancreas isn’t able to produce enough insulin to regulate blood sugar levels. Unfortunately, the reason behind this phenomenon is unknown, but research points to certain risk factors that can contribute to the development of the disease.
Type 2 Diabetes Risk Factors
The following conditions may increase your likelihood of developing type 2 diabetes:
- Being overweight or obese
- At age 45 or older
- Have a family history of diabetes
- Have high blood pressure
- Are not physically active
- Are African American, Alaska Native, American Indian, Asian American, Hispanic/Latino, Native Hawaiian, or Pacific Islander
- Have a low level of HDL (“good”) cholesterol, or a high level of triglycerides
- Have a history of gestational diabetes or gave birth to a baby weighing 9 pounds or more
- Have a history of heart disease or stroke
- Have depression
- Have poly cystic ovary syndrome (PCOS)
- Have dark, thick, and velvety skin around your neck or armpits
Type 2 Diabetes Symptoms
In a report by the CDC, it’s estimated that there are 84.1 million adults in the U.S. living with prediabetes. Prediabetes presents itself through higher-than-normal blood sugar levels, but not high enough to be considered a formal type 2 diabetes diagnosis. If left untreated within 5 or so years, however, prediabetes can develop into Type 2 diabetes.
High blood sugar isn’t the only indicator to diabetes. The early signs and symptoms one should look out for include:
- Urinating frequently
- Increased thirst
- Always feeling hungry
- Feeling very tired
- Blurry vision
- Slow healing of cuts and wounds
- Tingling, numbness, or pain in the hands or feet
- Patches of dark skin, usually in the armpits or neck
- Itching and yeast infections
- Unintended weight loss
- Irritability
- Cloudy thinking

Type 2 Diabetes Diagnosis
Your doctor may recommend a few different tests to measure your blood sugar levels. In general, the American Diabetes Association recommends getting screened for diabetes every three years after age 45. If you’re overweight and have a family history of diabetes, live a sedentary lifestyle, or if there are any other risk factors present, it’s recommended you get routinely screened as well.
A1C Test
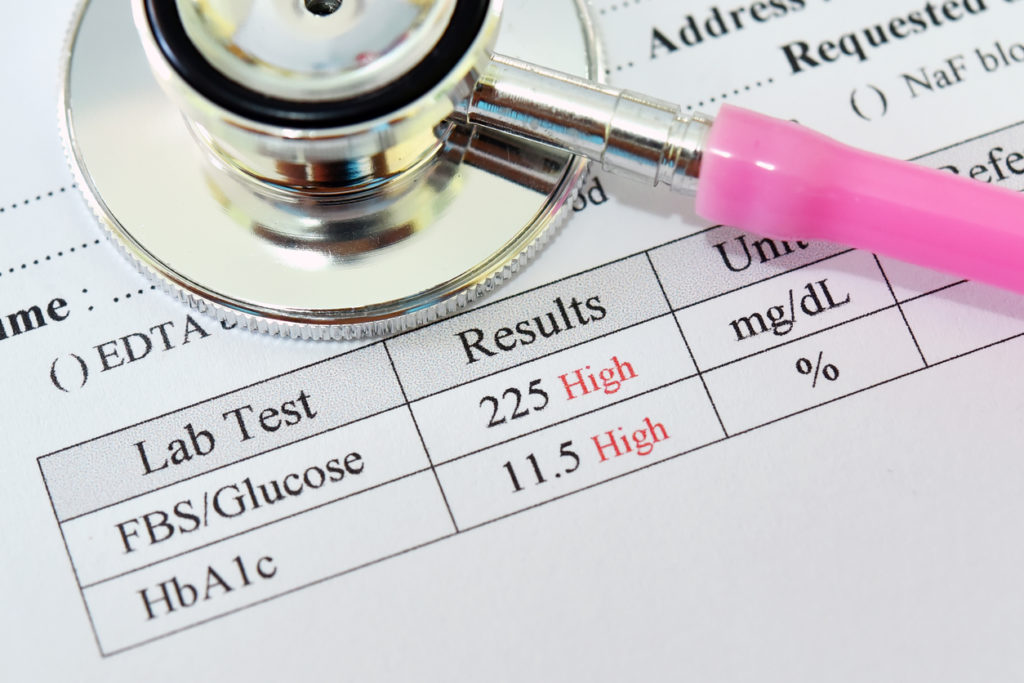
A common test that is used to identify type 2 diabetes is the glycated hemoglobin (A1C) test. The A1C test measures your average blood sugar level for the past two to three months, and what percentage of hemoglobin is coated with glucose (glycated). Hemoglobin is a protein in red blood cells that carries oxygen throughout the body. If your A1C test results fall between 5.7 and 6.4 percent, that’s an indicator for prediabetes. If the results are 6.5 percent or higher on two separate tests it indicates a formal type 2 diabetes diagnosis.
Fasting Plasma Glucose (FPG) Test
The preferred method for screening for diabetes, the fasting plasma glucose (FPG) test, measures your blood sugar levels after fasting for at least 8 hours. If you’re undergoing an FPG test, you’re not permitted to eat or drink anything (except water) for 8 hours or more. The test usually takes place first thing in the morning before breakfast to get an accurate result. Diabetes is diagnosed if the FPG test results in fasting blood sugar at or above 126mg/dL.
Random/Casual Plasma Glucose Test
As the name implies, this test is conducted by your doctor at random – at any given time in the day, regardless of when you ate your last meal. This is performed in the doctor’s office or clinic and is particularly useful for those who need a speedy diagnosis. A blood sample is taken from your finger to measure your random blood sugar level. A result of blood sugar falling between 140 and 199 mg/dL indicates prediabetes, while a level of 200 mg/dL or more results in a diabetes diagnosis.
Oral Glucose Tolerance Test (OGTT)
The oral glucose tolerance test (OGTT), while mainly used to diagnose gestational diabetes, can also diagnose type 2 diabetes. Like the FPG test, individuals need to fast for at least 8 hours before the OGTT test to ensure an accurate result. During the test, the technician or nurse will draw a blood sample to measure your fasting blood sugar level first. Following the initial fasting blood sugar test, you’ll drink about 8 ounces of a syrupy solution that has 75 grams of sugar. Since this test evaluates how your body responds to and handles sugar, your blood sugar level will be measured again two hours after drinking the solution. Like other tests, a blood sugar level of 200 mg/dL or higher may diagnose type 2 diabetes.
It’s important to note that tests results can vary, so getting a second opinion matters in identifying if you’re at risk, prediabetic, or have type 2 diabetes.
Type 2 Diabetes Treatment
Managing type 2 diabetes requires a combination of lifestyle modifications and medication to control your blood sugar level. Have a discussion with your doctor to identify the best treatment plan for you and your target blood sugar level. In addition, it’s crucial to managing the disease through regularly testing your blood sugar and keeping tabs on your symptoms.

Lifestyle changes you may have to make to help keep your blood sugar level in check include eating healthier foods, exercising, quitting smoking, and using dietary supplements when necessary.
It’s also common to prescribe those recently diagnosed with type 2 diabetes with an oral medication called metformin. Metformin (Glucophage, Glumetza, Riomet, Fortamet) is often prescribed at the lowest dose to start, since side effects can upset your digestive system. With metformin, most people see their blood sugar levels decrease in a few weeks. For some, metformin along with proper lifestyle changes is enough to manage their diabetes.
Other treatments include medications that can support your body in producing more insulin or improving your body’s sensitivity to insulin. Others can help manage blood sugar, lower the risk for heart disease, or support weight loss. All these factors can help you handle the disease and live a healthy life.
Ongoing Support
Living with diabetes can be managed in a number of ways, and there’s plenty of resources available to help. Consider enlisting some of these areas of support into your life so you can better control the disease:
- Dietitian: A dietitian can help you craft meal plans that are right for you.
- Endocrinologist: A doctor who specializes in diabetes, they can help you learn more about how to manage you case alongside your primary care physician as well.
- Diabetes Support Groups: Support groups can help you connect with others going through the same experiences with type 2 diabetes. You can find a diabetes support group near you through a simple Google search, or Defeat Diabetes Foundation provides a full list of support groups by state as well.
- Home Care Service: Having trouble managing your medications, or could use assistance around the house? Our team at Open Systems Healthcare can help. Learn more about our personal care services and find an office near you.
